© 2024 Abode Hospice and Home Health
All Rights Reserved
All Rights Reserved
When it comes to dealing with grief, there’s no one-size-fits-all approach. Everyone grieves differently, and grief can affect individuals, families, and a person’s entire social circle. The grieving process can be especially complicated for those who are homebound or on hospice with a terminal illness.
Creating a plan of care for home care or hospice patients must also incorporate grief. By including grief in an individual’s plan of care, we are able to meet the holistic needs of patients and support them throughout the process.
Home health services allow patients to comfortably remain living in their homes with the support of exceptional medical professionals. However, individuals with chronic conditions or recovering from an illness may also experience grief, especially during the early stages of adjusting to a new life.
Patients may grieve the loss of the life they once knew, which comes with a set of new emotions to tackle. After an injury, illness, or surgery, it can be difficult for patients to adjust to changes in abilities and personal freedoms/independence.

As we develop a plan of care for individuals receiving home health care, it is vital to consider this grieving process. By acknowledging this grieving process, home health professionals can actively support healing and find supportive ways to improve the mental wellness of these patients. It is important to remember that healing looks different for every patient, and no timeline can be associated with processing grief.
Hospice care is focused on supporting patients with terminal illnesses to be as comfortable and pain-free as possible. When an individual is put on hospice, grief can occur both personally and for family members. Many families of patients experience anticipatory grief before an impending loss. This type of grief can cause individuals to feel many unexpected emotions: fear, sadness, loneliness, anger, and more.
Coping with grief can look different for every patient and family member. What brings one person comfort may not help another.
Creating a personalized hospice care plan is one of the ways our hospice team can help support individuals and their families experiencing grief. From providing emotional support to additional resources, there are many ways hospice care can support grieving individuals.

To take things a step further, we offer a helpful bereavement program, which can support families during a difficult time in their lives. We provide one-on-one support, supportive phone calls and in-home support sessions to help each individual manage the grieving process and begin their healing process.
Whether you’re grieving a change in abilities or the loss of a loved one, each person’s grieving process is entirely unique. We incorporate grief into the plan of care for both home health and hospice patients. To learn more, contact us anytime to learn more about how our home health and hospice care can help support you and your loved ones through any stage of grief.
Watching someone you love suffer from Alzheimer’s or another memory debilitating illness is incredibly difficult, and it can be even more challenging to decide when it’s time to consider hospice care. Here, we are sharing five signs it may be the right time to consider the extra support of hospice care for an Alzheimer’s patient.
The Functional Assessment Staging (FAST) Scale is a tool used to determine if changes in a patient’s condition are related to Alzheimer’s disease or another condition. If due to Alzheimer’s, the changes will occur in sequential order. Alzheimer’s disease-related changes do not skip FAST stages.
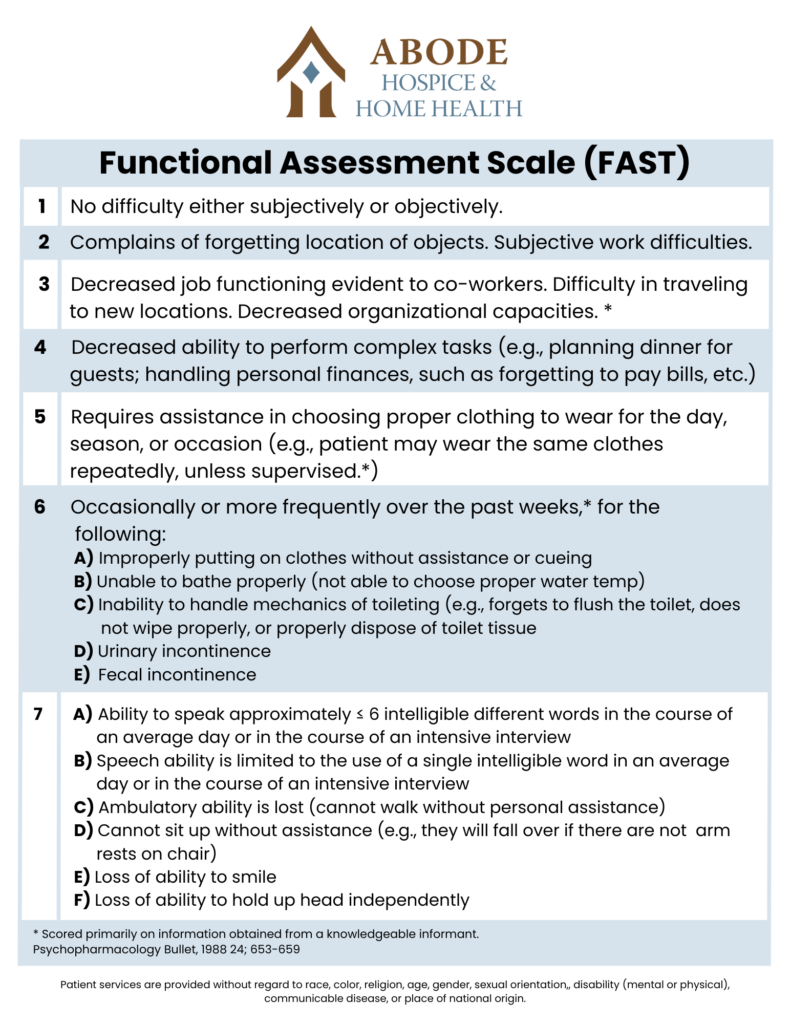
This means a person is no longer able to get around on their own. For example, they require assistance getting from room to room.
Without assistance, you may notice they put their shoes on the wrong feet or their day-time ‘street’ clothes on over their pajamas. They are also unable to bathe without assistance.
This includes urinary or fecal incontinence or both.
This may begin as the patient only saying 5-6 words per day and gradually reduce to only speaking one word clearly until they can no longer speak or communicate at all. This will also include the inability to smile.

Hospice care is for patients with a life limiting illness and a life expectancy of six months or less. The main focus is to manage pain and symptoms and ultimately keep the patient comfortable. When you choose hospice for your loved one, their care team can help you to understand what to expect in the final stages of Alzheimer’s. They will also provide support to you and the rest of your family throughout the end-of-life process.
If you would like more information on hospice care for Alzheimer’s patients, please contact us. We are here to answer any questions you may have.
This May, join us in celebration of America’s 4.4 million registered nurses who make a touching difference in the lives of patients and their families. Exceptional nurses often have a true passion for helping others, backed by compassion and empathy.
In honor of this month, we express our appreciation for home health nurses, hospice nurses, and nurses who work in the skilled nursing facilities that partner with us as hospice and home health providers.
Nurses make a profound impact in improving the quality of life of individuals in skilled nursing facilities, hospice care, and home health care. We invite social workers, medical professionals, and anyone who has been touched by a nurse to celebrate Nurse Appreciation Month with us. This is your reminder to thank your nurses and show you appreciate their “special touch”.

Nurses working in skilled nursing facilities serve a vital role in helping individuals get back on their feet after an injury or illness. While in rehabilitative nursing care, patients are supported by nurses who are committed to helping them improve their quality of life and regain strength during recovery.
Often, it is because of the support from nurses in rehabilitative nursing care that individuals can safely return to their homes for ongoing support from home health nurses. This allows individuals to continue recovering from the comfort of their own homes.
Throughout the month of May, we also recognize and show we appreciate the exceptional home health nurses that support patients in their homes. Home health nurses play a vital role in supporting an individual’s road to recovery as they strive to regain independence and autonomy in the home. Home health staff support the holistic health of individuals beyond physical care by also providing social and emotional support.
Hospice nurses have a special role in the lives of patients diagnosed with a terminal illness and their families. Nurses providing end-of-life care through hospice services help reduce unnecessary pain and suffering, making individuals as comfortable as possible in their final months or days of life. In addition, hospice nurses generously share their skills and compassion to provide supportive care that improves an individual’s quality of life, developing strong bonds with patients and their families.

Often, hospice nurses go above and beyond the call of duty, showing exceptional compassion for those nearing the end of their life. Not only do hospice nurses support an individual’s wishes, but they also provide support resources for family and friends during difficult times. Most families never forget the lasting impact the nurses made during an incredibly challenging period in their life.
Nurses in skilled nursing facilities, hospice care, and home health nurses demonstrate admirable qualities such as compassion, patience, and empathy. On behalf of our team and our partners, we honor the champions that have dedicated their careers to improving the lives of others. We couldn’t do it without you!
April 16 is National Healthcare Decisions Day (NHDD), designed to “inspire, educate, and empower the public and providers about the importance of advance care planning.” Being diagnosed with a terminal illness can be overwhelming for individuals and their families.
When diagnosed with a terminal illness, knowing where to turn next can be difficult. Furthermore, many people have misconceptions about hospice and when it should be introduced. This article will break down these common misconceptions surrounding hospice.

Hospice care is for people with a prognosis of 6 months or less if their disease runs its natural course. This type of care focuses on making those with a terminal illness as comfortable and pain-free as possible. Hospice care includes social, medical, emotional, and spiritual support. The goal of hospice care is to provide terminally ill patients the opportunity to live the last stages of their life with comfort and dignity.
Unfortunately, many common misconceptions surrounding hospice may prevent individuals from taking advantage of hospice’s many benefits. One common misconception is that “hospice is a place.” However, hospice can be provided wherever a patient is located, which sometimes includes right in their home. Another common misconception is that “hospice is giving up,” but this could not be further from the truth. Many people end up living longer in hospice or sometimes graduate from hospice and no longer qualify.
While on hospice, patients can choose to keep their primary care physician (PCP). Hospice care staff will work with your PCP and other healthcare professionals to provide collaborative care. Some people also avoid hospice care because they feel it is “pointless” as their illness is terminal. While curative treatment may no longer be an option, that doesn’t mean other efforts serve no purpose. Living with a terminal illness can often cause individuals lots of pain. That’s why hospice care is a great option, as it serves to make individuals as comfortable and pain-free as possible. These supportive measures are key in the final stages of a person’s life.

Instead of waiting until the very end to receive hospice care, individuals with a terminal illness can fully benefit from hospice care sooner rather than later. Others may decide to stop hospice to try another experimental treatment. Hospice can be designed to work for each patient’s individual needs. With hospice, you or your loved one are in the “driver’s seat” of your own healthcare decisions.
Hospice care is a great healthcare option when curative treatment is no longer viable. Furthermore, hospice isn’t just for the last days or weeks of life. Hospice can support individuals for several months. Don’t let the common misconceptions surrounding hospice hold you or a loved one back from receiving supportive care.
Our care team supports patients in determining their own goals of care during the final stages of their illness. Our hospice care service focuses on comfort, support, quality of life, and education. Contact us today to discuss your questions and personal needs.
Did you know that March is National Kidney Health Awareness month? Each March helps raise awareness about promoting good kidney health and highlights how home health and hospice care can help support those with kidney disease.
Sadly, kidney disease is often referred to as a silent disease that can manifest without the presence of many symptoms in its early stages. Often, individuals diagnosed with Chronic Kidney Disease (CKD) are unaware of their condition until it has advanced to later stages.
Before you can understand ways to protect your kidneys, it’s vital to understand the critical function of kidneys in the body. Kidneys help regulate the body’s fluid levels, filtering out waste and toxins from the bloodstream. In addition, your kidneys release an essential hormone in blood pressure regulation. Kidneys also serve many secondary purposes, such as activating Vitamin D to maintain healthy bones and keeping blood minerals like potassium and sodium in the correct balance.
With all these vital functions in mind, it’s clear that protecting your body’s kidneys is crucial to good health.
Promoting good kidney health starts with protecting your kidneys. First and foremost, drinking enough fluids daily keeps your kidneys functioning effectively. Adults who do not have a diagnosed kidney condition should drink about 9 to 13 cups of fluid daily, according to the National Kidney Foundation.
Your diet and lifestyle are also quite important to maintaining good kidney health. By eating a well-rounded diet and maintaining a healthy body weight, you’ll help protect your kidneys from many factors that contribute to kidney damage. Aim to get at least 30 minutes of physical activity every day. It may take time, but developing a regular exercise routine can go a long way in helping support your overall health, as well as your kidney health.
Drinking too much alcohol can also wreak havoc on your kidneys and put them at risk for kidney disease. Consume alcohol in moderation. In addition, smokers are at an increased risk for kidney disease.
If you or a loved one has received a kidney disease health diagnosis, there is help. Our team offers supportive in-home services for individuals in need. We review services for individuals on dialysis on a case-by-case basis. Some individuals can continue dialysis treatments while also receiving supportive home health or hospice services. To learn more about how home health and hospice services can help you or a loved one, speak to a representative to discuss your unique situation.
Interested in learning more about the home health or hospice services available to individuals receiving dialysis? Contact us today.
Each year, Patient Safety Awareness Week (PSAW) is recognized to remind healthcare staff of the importance of promoting patient safety practices. Whether you’re a Nurse, Certified Nursing Assistant, or another type of healthcare professional, the steps you take daily can go a long way in keeping your patients safe.
From preventing choking hazards to simple fire prevention techniques, check out these five preventative measures you can implement to keep your patients safer.

Elderly patients or patients in hospice are at an increased risk of falls, which can be caused by age-related loss of muscle mass, balance problems, cluttered environments, and so much more. While you’re likely already familiar with general fall risk precautions, one easy tip that is often forgotten is to ensure that a patient’s living area is adequately lit. According to the Centers for Disease Control (CDC), falls are usually caused by a combination of risk factors. The fewer risk factors a person has, the less their risk for falls is. As a healthcare professional, consider these ways to help encourage fall prevention for your patients:
Another vital part of keeping your patients safe is understanding oxygen safety and fire prevention techniques. Remind your patients on oxygen that oxygen is extremely flammable. Therefore, provide patient education and remind patients of the dangers of smoking near an oxygen tank. Furthermore, all patients who smoke should be made aware of the designated smoking areas around your healthcare facility.
For home care patients, healthcare professionals can also help support fire prevention by helping their patients perform regular smoke detector tests or replace batteries.
Another easy way to keep your patient safe is to follow proper eating protocols to prevent choking. Bed-ridden patients may wish to eat lying down. However, this poses a serious choking hazard. Before feeding a patient or giving them a meal, ensure they sit upright. After eating, patients should remain upright for at least 30 minutes to prevent aspiration. Any patient that has difficulty swallowing should take small bites with sips of liquids in between.

Most healthcare professionals already know that frequent repositioning is an important step to prevent bed sores. However, adequate nutrition is another essential component to help reduce the risk of bed sores. Research studies suggest a clear correlation between nutritional deficiencies and an increased risk for pressure ulcers. Healthcare professionals and dietary department workers should pay close attention to their patients’ diets, helping to ensure they have a well-rounded diet with nutrient-dense foods. For patients with poor appetite, supplemental nutrition may be needed to help obtain proper nutrition and prevent bed sores.
When it comes time to transport a patient, healthcare professionals have many things to remember. Especially for patients who need help to ambulate several times throughout the day, it can be easy for healthcare professionals to forget the most important safety precautions for safe ambulation. As you prepare a patient for transport, ensure that they have the proper footwear to prevent falls. Standard socks are not proper footwear. Instead, patients should have non-slip shoes or socks on. Taking an extra moment to ensure your patient has adequate footwear is a simple and effective way to ensure they are safely transported.
Patient safety is our utmost priority. To support this year’s Patient Safety Week, try implementing these five simple ways to keep your patients safe. Whether you see patients in a home setting or an assisted living facility, these tips can help reduce fall risk, prevent bed sores, eliminate choking hazards, and reduce fire hazards.
Some older adults and people with serious illnesses, unfortunately, experience the end of life in certain healthcare settings that do not align with their desired wishes. If you have a serious illness or are a caregiver of someone planning end-of-life care, knowing the difference between palliative care and hospice care can help you make an informed decision when the time comes to transition to one of these healthcare settings.
Palliative care is a form of care that focuses on improving your quality of life and that of your family when you are living with a serious illness. It focuses on your whole-person health rather than only on your condition. If you are receiving palliative care, your treatment plan may focus on reducing symptoms of your illness and on improving secondary conditions such as depression, sleep deprivation, and side effects of medications.
Palliative care may be given in various healthcare settings, such as at the hospital, a residential care facility, or your home. Anyone can receive this type of care regardless of age or the severity of their condition.
If you receive palliative care, you may work with and be treated by various healthcare professionals, including doctors, nurses, social workers, pharmacists, physical therapists, counselors, and nutritionists. If you need spiritual care, your palliative care team may even include a chaplain. The healthcare professionals that make up your palliative care team will depend mainly on your recovery needs and level of care.
Studies show that palliative care offers many benefits, including:

Hospice care focuses on improving your comfort and quality of life when you are nearing the end of your life. This type of care is usually given in circumstances in which an illness continues to progress despite treatment or when the patient chooses not to receive certain treatments. Hospice care is similar to palliative care in that it provides comfort care and support for the family. However, treatments are not given to improve the illness.
Like palliative care, hospice care can be given in many different healthcare settings, though it is most frequently given at your home, where you can be most comfortable and spend quality time with your loved ones. In addition, it is typically given when your healthcare provider believes you have no more than six months to live. Some benefits of hospice care include 24/7 access to nurses and healthcare workers who can address and relieve symptoms and side effects and access to medical equipment and medications that can reduce your discomfort.
Many of the same types of healthcare professionals that make up a palliative care team will also be part of your hospice care team. This includes doctors, nurses, social workers, chaplains, and volunteers who dedicate their time to giving you the support you need and making you feel as comfortable as possible during your final months.
To be eligible for hospice care, you will discontinue aggressive treatment efforts to combat your terminal illness (such as experimental surgeries, aggressive chemotherapy, or other treatments that require prolonged hospitalization and recovery). However, you may continue to receive treatments for other conditions, such as antidepressants to treat depression or insulin medicines to control Diabetes.
Comfort care and end-of-life care are both terms that describe the type of care you receive when you are near the end of your life and are no longer receiving treatment for your illness. It is highly similar to palliative care in providing you with whole-person care that focuses on your physical, social, emotional, and spiritual health. Comfort care and end-of-life care may include palliative care or hospice care, or a combination of both.
Sometimes, palliative care is given as part of hospice care, and both types share many similarities. For instance, the goal of both palliative and hospice care is to improve your quality of life and help you find relief from painful and severe symptoms and side effects of treatment. Both types of care also focus on whole-person health. However, there remain many differences between palliative care and hospice care.
Some of these differences are:

You may want to consider palliative care if you or your loved one has a serious illness or chronic condition that requires long, intensive care or that causes severe physical symptoms and/or emotional distress. For example, cancer, heart disease, AIDS, and kidney failure are some of the many conditions that can benefit from palliative care.
Additionally, palliative care may benefit you if you:
A person may transition from palliative care to hospice care if their doctor thinks they have no longer than six months to live. Sometimes, it can be difficult for doctors to predict exactly how long it will take for a particular disease to run its course or how long a person has left to live if their health is in decline. In these circumstances, it’s important to consider how transitioning to hospice care could improve your quality of life during your final months.
According to the National Library of Medicine (NLM), doctors should strongly consider referring chronically ill patients to hospice care if they spend more than half their time in bed, are unable to function efficiently, and are experiencing both physical and psychological distress. The NLM adds that hospice referrals are usually necessary when the patient’s condition has progressively declined to the point that their highest priority is to take control of their healthcare and achieve the greatest possible comfort in their homes as they near the end of life.
Talk to your doctor if you think you may need hospice care but aren’t sure when you should transition out of palliative care. Your doctor can talk to you at length about your options and the benefits of transitioning to hospice care based on your condition and unique circumstances.
Taking advantage of hospice care as soon as it’s needed could result in access to quality care and lots of extra quality time to spend with your loved ones. Additionally, studies show that patients who plan their care in advance are more likely to be satisfied with their care, given how they can make decisions that align with their end-of-life wishes.
Consult with your healthcare provider if you or your loved one is interested in learning more about palliative care or hospice care. Your doctor can refer you to a palliative or hospice care specialist who can answer all your questions and help you determine which of these services may be more ideal.
Palliative care and hospice care are covered by many major health insurance providers, including Medicare. The exact benefits covered will vary based on your health plan. Benefits covered may include medical equipment and supplies, skilled nursing care, bereavement support, and medications to provide comfort, among many others.
Abode Hospice & Home Health has resources for home health and hospice services throughout the United States. Specialty services we offer include diabetes care, orthopedics, and pain management. Call us today to learn more about our many home healthcare services.

It’s time to speak up about breast cancer, and the month of October is dedicated to doing just that. As the most common form of cancer, it’s likely that someone in your life whom you care for deeply has been diagnosed with breast cancer. Given how prevalent breast cancer is and the repercussions it has on individuals and families affected, this month is a time to rally together and raise awareness about it.

In the United States, more women die from breast cancer every year than any other form of cancer. It’s currently estimated that 1 in 8 women in their lifetime will be diagnosed with an invasive form of breast cancer. Two of the greatest risk factors of getting breast cancer are female gender and older age, though men and younger women can get it as well. The statistics are alarming, and a diagnosis can feel daunting and isolating, whether it’s yourself or a loved one or family member who is receiving it. Fortunately, breast cancer research continues to thrive, which has led to improvements in screening processes and treatment success. These improvements have been given some of the credit for the slightly decreased death rate from breast cancer over the past several years. In order to take further advantage of the strides we’ve made in battling breast cancer, we must continue to educate our communities about the screenings and treatments available.
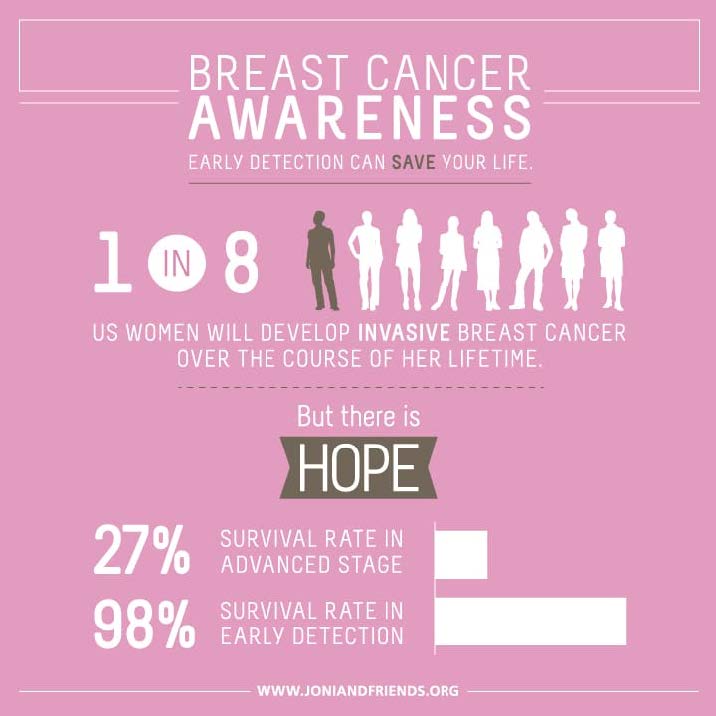
While there is no way to guarantee prevention of breast cancer, it is recommended that all adult women perform a breast self-exam monthly. This is a great way to self-monitor for any changes or abnormalities that may occur in the breast tissue. As you age, this becomes an even more important habit as age is one of the main risk factors. It is important to note that not every growth or lump felt in the breast tissue is a cancerous mass. Some non-cancerous masses are abnormal but do not grow outside of the breast tissue. While these lumps do not innately pose a risk, some of these growths can increase a women’s risk of getting breast cancer down the road. Any abnormality or change in your breast tissue that you notice or feel should be examined by a health professional immediately. Just under half of women diagnosed with breast cancer were diagnosed after noticing a lump during a self-exam, so the importance of this routine cannot be overlooked. In addition to regular self-exams, maintaining a healthy weight through exercise and a nutritious diet is another important way to reduce your risk of breast and other cancers.
Should you receive a diagnosis of breast cancer, take the time to find a team of doctors whom you are comfortable with and trust with your care. This team can include an oncologist, or cancer doctor, a surgical oncologist, a radiologist, a case worker, a registered dietician who specializes in cancer nutrition and possibly several other specialty providers. These individuals will be with you, alongside your personal support system, to make sure you receive the best care available from diagnosis on. Treatments and interventions will differ depending on the type of breast cancer you are diagnosed with and your doctors will help you navigate all of the options and should use their expertise to recommend the best course of action. Make sure you feel comfortable asking questions and engaging in your treatment plan. Your providers have the knowledge and the skill sets to provide excellent care, but it is just as important that you feel included in the decisions being made and prepared for the treatment road ahead.

Whether you are young, old, male, female, part of a high-risk category or not, it is our shared efforts in spreading awareness this month of October and all months following that will successfully raise awareness, education, and resources about breast cancer to every individual diagnosed and every family and friend supporting them. As a society working together, it is within our reach to decrease breast cancer diagnoses within our communities and to improve the outcomes and survival rates of those diagnosed.
National Breast Cancer Foundation, INC.